Advice for chiropractors
As musculoskeletal specialists in primary care, chiropractors can play a key role in reducing the unacceptable 8.5-year delay to diagnosis in axial spondyloarthritis (axial SpA).
Jonathan Field is Chair of the Pain Faculty at the Royal College of Chiropractors and Clinical Lead for the Back Active NHS Community Physical Therapy Service in North Hampshire. Below, Jonathan describes how to recognise and refer patients with suspected axial SpA.
For every 100 patients attending their service, Jonathan and his team identify approximately 5 patients who meet the criteria for suspected inflammatory spinal disease. Those individuals at risk are identified using the axial spondyloarthritis referral tool, developed jointly by the Royal College of Chiropractors and the Institute of Osteopathy, in collaboration with NASS. This tool has been validated by the Royal College of GPs and the Chartered Society for Physiotherapy.
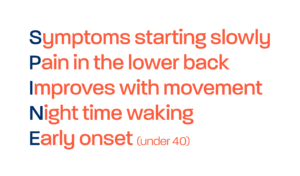
The referral tool is available below and is comprised of the following:
We recommend reading through the referral template and guidance and utilising this next time a patient presents to you in clinic with chronic back pain.
For more details on how Jonathan and his team identify patients with axial spondyloarthritis in their service, please watch the video above, or read the associated blog below.