Recognising axial SpA: 5 top tips
1.CHRONIC BACK PAIN WITH ONSET AGED <45 YEARS? THINK AXIAL SPA
Axial SpA isn’t as rare as one might think – approximately 1 in 200 individuals in the UK are living with this condition. It is important to move away from just thinking of axial SpA solely as ankylosing spondylitis, identified by X-ray changes to the spine, and instead consider the wider net of people with non-radiographic axial spondyloarthritis also. These patients may present with a variety of symptoms – but the key feature is chronic back pain with onset aged <45 years.
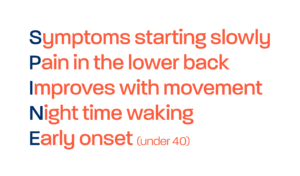
2. RECOGNISE INFLAMMATORY BACK PAIN
Physiotherapists are often brilliant at recognising what isn’t mechanical back pain. But it is good to remember that inflammatory back pain isn’t as simple as back pain that gets better with exercise and worse with rest. A lot of cases of suspected axial SpA picked up in clinic may instead be experiencing night pain or waking in the second half of the night. Similarly, presentations of alternating buttock pain should always raise suspicion of an inflammatory condition.
3. RECOGNISE THE EXTRA-ARTICULAR MANIFESTATIONS OF AXIAL SPA
Axial SpA is associated with a range of extra-articular manifestations, or EAMs, including acute anterior uveitis, psoriasis, and inflammatory bowel disease (ulcerative colitis and Crohn’s disease) – conditions associated with the eyes, skin, and bowels, respectively. Dactylitis and enthesitis are also EAMs of axial SpA, and these are terms that you need to be familiar with. Blood tests can also build up a clinical picture of potential axial SpA. For example, HLA-B27 is not diagnostic of axial SpA, but a large proportion of people with axial SpA will be positive for this blood test. Approximately 8% of white western Europeans carry this gene, in comparison to 75-90% of individuals with axial SpA. However, only about 1 in 15 people who are HLA-B27 positive go on to develop the condition. Over 100 genes are now thought to be involved in axial SpA, with HLA-B27 believed to be responsible for no more than 25-30% of the genetic risk.
4. QUESTION EARLY MORNING STIFFNESS OF THE JOINTS/ SPINE
Early morning stiffness is in itself, subjective. However, we know that joint stiffness is indicative of inflammatory changes in the body. Try to probe and listen to the person’s qualitative recollection of that morning stiffness, as it will likely give you an indication of whether this stiffness is inflammatory in nature.
5. KNOW YOUR LOCAL RHEUMATOLOGY PATHWAYS
Contact, reach out and link with your local rheumatology services. Find out what the appropriate referral pathways are, and what they would like/ not like First Contact Practitioners to do. For example, they may prefer you to refer any patient with potential undiagnosed axial SpA on to rheumatology, rather than performing any further tests or investigations in primary care, e.g. blood tests for HLA-B27. This is applicable not just for axial spondyloarthritis, but for all rheumatic conditions.