How to recognise and manage axial SpA in patients with IBD
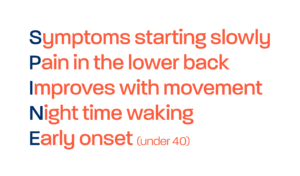
The key symptoms to look out for are:
- Lower back pain
- Pain particularly prevalent in the morning
- Pain that radiates into the buttocks
- Morning stiffness of >30 minutes
- Pain that is responsive to NSAIDs (although of course, not often used in IBD) – another good indicator of inflammatory lower back pain
The key imaging diagnostic used by rheumatologists currently is an MRI of the sacroiliac joints. If there is evidence of sacroiliitis on MRI and patients are also experiencing axial SpA symptoms, then referral to rheumatology is recommended. Rheumatology specialist input to conduct the MRI is recommended in most cases, as a specific axial SpA MRI protocol should be used, and correct interpretation can be challenging in the context of axial SpA. Therefore, in most cases, NASS would advise considering referral of all individuals with IBD and chronic (>3-months) back pain with onset before the age of 45 straight to rheumatology. This can often be done via an internal tertiary referral pathway.
Joint management between gastroenterology and rheumatology is key and will give the best outcomes for patients. However, if that is not possible, rheumatological input is still critical when considering changing medications.
IBD and axial SpA patients respond to the same medications in a lot of cases – for example, the anti-TNFs. Indeed, presence of sacroiliitis or spondyloarthritis can be a trigger for using anti-TNFs to manage both IBD and potential spondyloarthritis symptoms. However, it is important to note that some biologics have differential effects on the two types of inflammation. For example, the IL-12/IL-23 inhibitors such as ustekinumab are not effective for axial SpA but are effective for Crohn’s disease. Similarly, IL-17 inhibitors are effective for the management of axial SpA, but not IBD. And indeed, even for anti-TNFs, doses differ between specialties. Hence, the importance of joint gastroenterology and rheumatology consultation to provide the optimal medication.
Good communication between gastroenterology and rheumatology is key when considering diagnosis and management of spondyloarthritis in IBD. This communication and joint decision making will ultimately deliver the best results for patients.