Dr Daniel Murphy is GP Principal at Honiton Surgery in Devon, Medical Advisor to NASS, as well as a Staff Grade Rheumatologist at Royal Devon & Exeter Hospital.
Daniel provides an overview of the importance of improved diagnosis in axial SpA, in addition to providing tips for recognising axial SpA in general practice.
Top tips for recognising axial SpA in general practice
1. LISTEN TO YOUR INTUITION
Axial SpA is a rare cause of a common problem: chronic back pain. As GPs, we are experts at assessing problems quickly, and picking out those key symptoms to make an efficient management plan. The first tip is listen to your intuition: Is there an alarm bell to suggest that the back pain doesn’t seem mechanical? And if that’s the case, ask more questions to determine if axial SpA could be the cause.
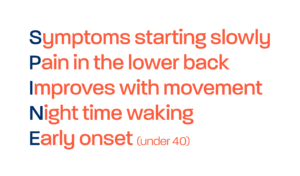
2. ASK 5 KEY QUESTIONS: KNOW THE HALLMARK FEATURES OF INFLAMMATORY BACK PAIN
If a patient answers yes to 4 or more of the following 5 questions, they have an approximately 80% chance of having inflammatory back pain.
- Did back pain start before the age of 40?
- Was the onset of pain gradual?
- Does the pain get better with exercise?
- Does the pain get worse, or not improve, with rest?
- Does the back pain cause waking in the second half of the night, requiring the individual to move around before feeling better and being able to fall asleep?
3. KNOW THE EXTRA-ARTICULAR MANIFESTATIONS OF AXIAL SPA
Axial SpA is associated with a range of extra-articular manifestations, or EAMs, including acute anterior uveitis, psoriasis, and inflammatory bowel disease (ulcerative colitis and Crohn’s disease). Dactylitis and enthesitis are also EAMs of axial SpA. Presence or prior bouts/ history of these conditions could indicate that a patient’s back pain is more likely to be inflammatory or axial SpA related. A family history of the above conditions, or of spondyloarthritis specifically, should also be considered.
4. INFLAMMATORY BACK PAIN? REFER TO RHEUMATOLOGY
Although the presence of EAMs can raise clinical suspicion of axial SpA, even without the presence of EAMs, presence of inflammatory back pain should indicate direct referral to rheumatology, to ensure the best outcome and treatment for patients.
Know your axial spondyloarthritis features, ask the appropriate questions, and refer early to rheumatology. This way, we can really help reduce delay to diagnosis in these conditions, to ultimately improve outcomes for our patients.