How to recognise & refer axial spondyloarthritis in the osteopathy clinic
A recent NASS survey indicated that 21% of people with axial SpA reported seeing an osteopath prior to being diagnosed.
However, recognising axial SpA can be challenging. There are a range of different symptoms associated with axial SpA, many of which may be intermittent, and the physical examination is often unremarkable. Therefore, osteopaths need to be knowledgeable in the various features of axial SpA, and screen for them regularly – with emphasis on historic symptoms, as well as current.
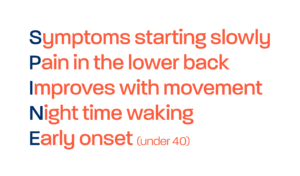
Symptoms of inflammatory back pain are key:
- Back pain with onset aged <45 years, pain lasting >3 months
- Waking in the second half of the night with pain
- Early morning spinal stiffness lasting >30 minutes
- Back pain/stiffness improves with movement, but not with rest
- Alternating buttock pain – usually relating to the sacroiliac joints
Screening for the extra-articular manifestations of axial SpA is also important:
- Psoriasis of the skin
- Enthesitis – inflammation of the entheses, the sites where tendons or ligaments insert into the bone, may present as aching or pain in the heel
- Uveitis – red, painful inflammation of the eyes
- Inflammatory bowel disease – Crohn’s or ulcerative colitis
- Dactylitis – inflammation of the finger and toe joints
Osteopaths should also ask if patients have a first degree relative with spondyloarthritis.
Some groups of patients have a longer delay to diagnosis of axial SpA. So it is important to screen regularly. Particularly for women, people who already have a diagnosis of fibromyalgia, and people with hypermobility.
If a patient has a number of symptoms of axial SpA, you can use the free online SPADE tool (http://www.spadetool.co.uk/) to input their symptoms and create a graph showing the likelihood that the patient has axial SpA. Osteopaths can use this in conjunction with the NASS referral template letter, to refer directly to their GP for the correct investigations, or onward referral to rheumatology.
The referral template was developed jointly by the Royal College of Chiropractors and the Institute of Osteopathy, in collaboration with NASS. And has been validated by the Royal College of GPs and the Chartered Society for Physiotherapy.
The referral tool is available below and is comprised of the following:
We recommend reading through the referral template and guidance and utilising this next time a patient presents to you in clinic with chronic back pain.