READ HERE
The Role of Early Treatment in the Management of Axial Spondyloarthritis: Challenges and Opportunities
Mauro, D., Forte, G., Poddubnyy, D. et al. The Role of Early Treatment in the Management of Axial Spondyloarthritis: Challenges and Opportunities. Rheumatol Ther (2023). https://doi.org/10.1007/s40744-023-00627-0
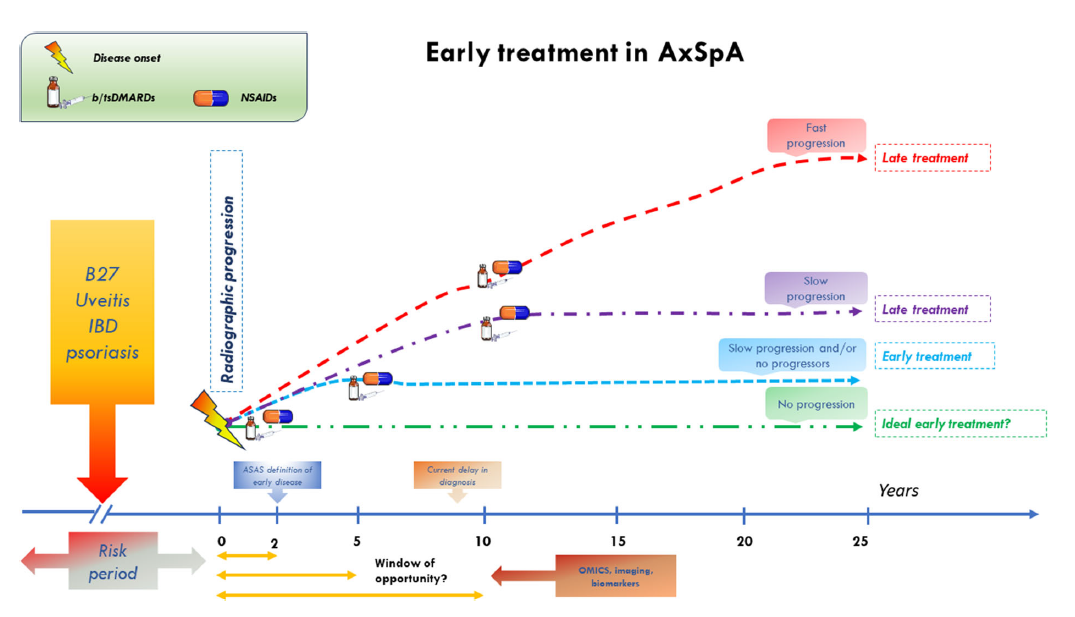
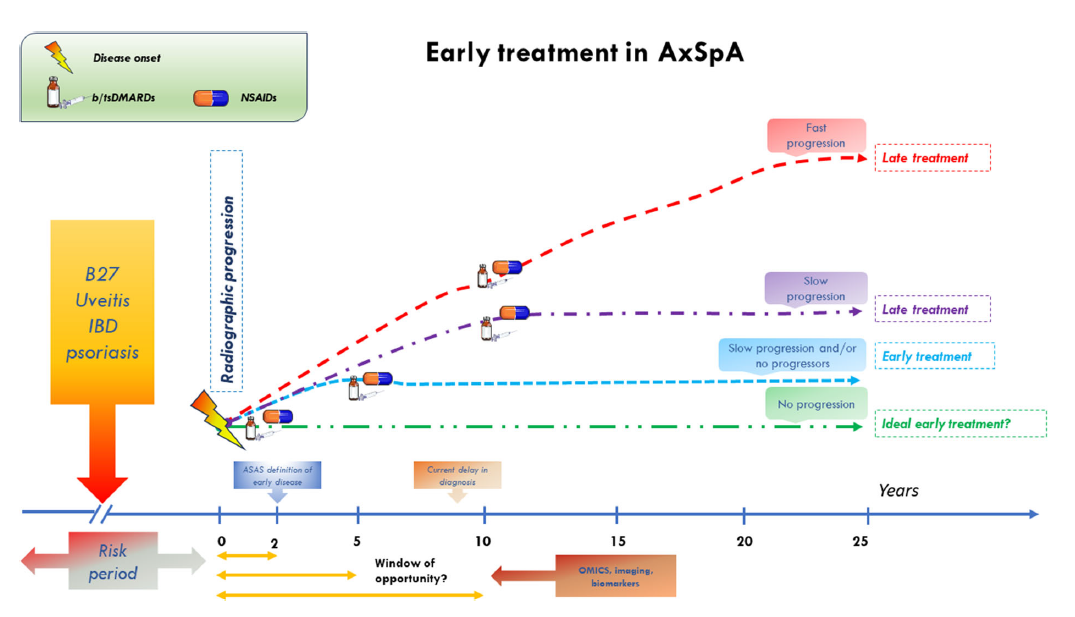
ABSTRACT: Axial spondyloarthritis (axSpA) is a chronic, inflammatory rheumatic disease that primarily affects the axial skeleton, often inflicting severe pain, diminished mobility, and a compromised quality of life. The advent of Assessment of SpondyloArthritis international Society (ASAS) classification criteria for spondyloarthritis (SpA)
have enabled the classification of patients with axSpA in the non-radiographic stage but poorly perform if mistakenly used for diagnostic purposes. Despite notable progress in early diagnosis facilitated by referral strategies and extensive magnetic resonance imaging (MRI) utilization, diagnostic delays persist as a concerning issue. This underscores the urgency to narrow the diagnostic gap and highlights the critical role of early diagnosis in mitigating the long-term structural damage associated with this condition. Research into the impact of nonsteroidal anti-inflammatory drugs (NSAIDs) and biologic disease-modifying antirheumatic drugs (bDMARDs) on inflammatory symptoms and radiographic progression has been extensive. A compelling body of evidence suggests that early intervention leads to superior disease outcomes. However, most of these studies have centered on patients with established diseases rather than those in the early stages. Consequently, findings from studies on early pharmacological intervention remain inconclusive, and the
potential for modifying the disease trajectory is still debatable. Without precise data from clinical trials, insights from basic science regarding the pathogenic mechanisms might point toward potential targets that warrant early intervention in the disease process. This review underscores the urgency of early diagnosis and intervention in axSpA, highlighting ongoing research gaps and the need for further exploration to improve patient outcomes.
———————————————————————
READ HERE
Diagnostic delay in axial spondyloarthritis: A lost battle?
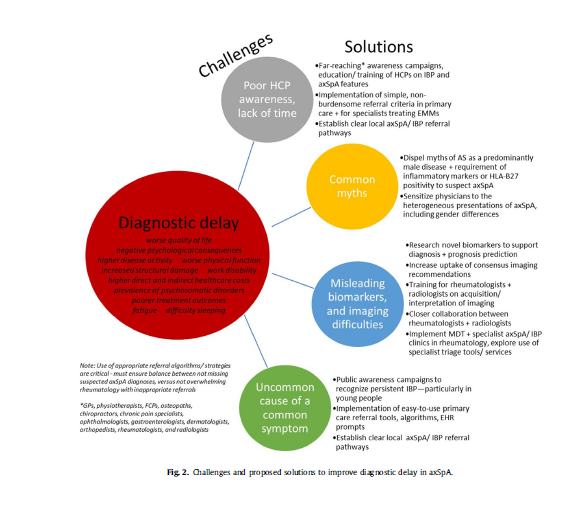
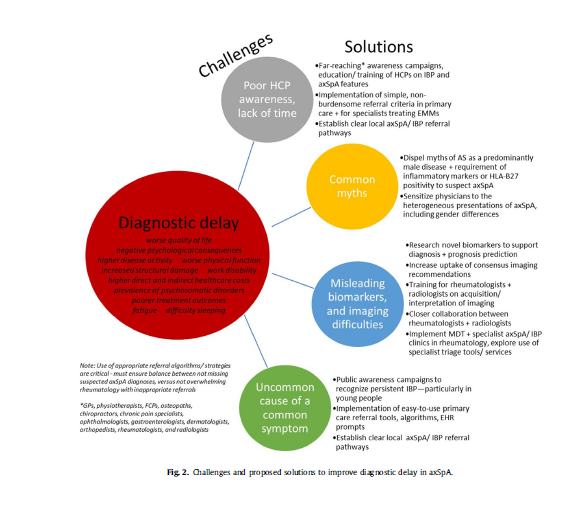
Abstract: Diagnostic delay in axial spondylarthritis (axSpA) remains an unacceptable worldwide problem; with evidence suggesting significant
detrimental impact both clinically on the individual, and economically on society. There is therefore, a need for global action across various healthcare professions that come into contact with patients living, and suffering, with undiagnosed axSpA. Recent estimates of the median diagnostic delay suggest that globally individuals with axSpA wait between 2 and 6 years for a diagnosis – revealing a clear benchmark for improvement. This timespan presents a window of opportunity for earlier diagnosis and intervention, which will likely improve patient outcomes. This review describes the current diagnostic delay as estimated across countries and over time, before presenting evidence from published strategies that may be implemented to improve this delay across primary and secondary care, including for specialties treating
extra-musculoskeletal manifestations of axSpA (ophthalmology, gastroenterology, dermatology). Ongoing campaigns tackling delayed diagnosis in axSpA are also highlighted.
Summary: Recent estimates of median diagnostic delay suggest that globally, an individual with axSpA will wait between 2 and 6 years for a diagnosis. This time presents a window of opportunity for earlier diagnosis and earlier intervention; which would likely have a profound impact clinically, on the individual, and potentially societally in terms of work productivity and healthcare cost savings. There are many proposed/published strategies for improving diagnostic delay in axSpA, which require further testing in future research, across different healthcare settings. Simple, non-burdensome strategies or automated prompts via EHRs will be key. Rheumatology services should work directly with local service providers in primary (such as GP practices and musculoskeletal interface services, physiotherapy services) and secondary care (orthopedics, ophthalmology, gastroenterology, dermatology, radiology) to establish clear referral criteria and pathways for suspected axSpA, appropriate to the local setting. Barriers to improved diagnosis include lack of healthcare professional awareness of axSpA
features, in addition to a lack of time/incentive to adopt proposed screening tools and strategies, highlighting the need for further robust data-driven evidence and national endorsement of these strategies to support/improve adoption. In coming years, it will be critical to assess the impact of recently introduced national, regional, and local initiatives and campaigns, to provide evidence for their impact on diagnostic delay and the individual journey for the patient. Although diagnostic delay in axSpA remains a global problem in rheumatology, it is not a lost battle. As clinicians, it is therefore of utmost importance to strive for improved education of HCPs across both primary and secondary care;
to engage with initiatives/campaigns to improve diagnostic delay; and to advocate for the testing and implementation of published referral strategies, recommendations, and quality standards, to ultimately improve the lives of patients.
Practice points:
- Delayed diagnosis in axSpA remains an extensive worldwide problem; recent estimates of the median diagnostic delay suggesting that an individual with axSpA will likely wait between 2 and 6 years for a diagnosis
- Evidence suggests that earlier identification and referral of suspected axSpA and the resultant earlier diagnosis and treatment, would likely improve both clinical outcomes for the individual and economic outcomes for the society
- Widespread implementation of education, training and simple non-burdensome referral strategies/prompts (within primary care and specialties treating EMMs) are recommended to improve diagnostic delay in axSpA
- Rheumatology services should work directly with local service providers in primary (such as GP practices and musculoskeletal interface services, physiotherapy services) and secondary care (orthopedics, ophthalmology, gastroenterology, dermatology, radiology) to establish clear referral criteria and pathways for suspected axSpA, appropriate to the local setting
———————————————————————————————————————————————————————-
READ HERE
A Survey of Diagnostic Delay in Axial Spondyloarthritis across two National Health Service (NHS) Rheumatology Services
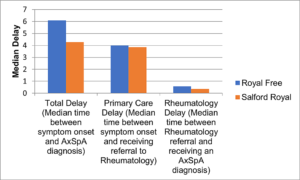
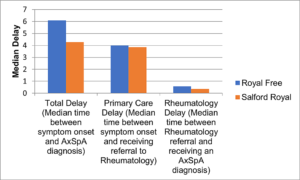
Introduction: Diagnostic delay is an ongoing challenge in axial spondyloarthritis (axial SpA). A recent, comprehensive literature review has found a mean average of 8.7 years of delay between symptom onset and formal diagnosis in the United Kingdom (UK). The primary aim of this study was to identify delays to diagnosis experienced by patients with axial SpA under the ongoing care of two urban National Health Service (NHS) rheumatology services. The secondary aims were (a) to count healthcare professional (HCP) interactions after symptom onset but prior to the diagnosis, (b) to compare our data to published delay to diagnosis research and (c) to explore contributing factors locally and the variation between the two UK rheumatology services. Results:
Those completing the survey formed a cohort of 106 participants with an established diagnosis of axial SpA who attended the axial SpA services at either Royal Free NHS Foundation Trust or Salford Care Organisation, Northern Care Alliance NHS Foundation Trust. The mean time from the onset of symptoms to the diagnosis of axial SpA was similar across centres despite the differences in demographics, with Royal Free at 5.72 years and Salford Royal at 5.96 years. When reviewing via median diagnostic delay, there was a notable difference with Royal Free at 6.09 years and Salford Royal at 4.27 years.
Across the two sites, between the onset of symptoms and the diagnosis of axial SpA, 90% of the participants saw a general practitioner (GP), of which 63% of the patients saw a GP 1-5 times, 23% saw 5-10 times and 14% saw more than 10 times. Many participants also saw other HCPs, including physiotherapists, other manual therapists and hospital specialists prior to diagnosis. In addition, 32% saw one other HCP, 18% two other HCPs, 9% three, 7% four and 2.7% five other HCPs prior to diagnosis. Close to 80% of the patients stated that they had received adequate axial SpA education at diagnosis, and 76% of the patients were aware of who to contact in the event of a flare. Conclusions: These data highlight that the mean average time to diagnosis for both trusts was between five and six years, somewhat lower than the 8.7-year national UK average. However, despite being specialist centres, these data are a long way from the National Axial Spondyloarthritis Society (NASS) “Gold Standard” of one year time to diagnosis. The contributors to this include lack of HCP and community awareness about axial SpA, its recognition and appropriate onwards referral. There is a need for concerted ways of working for the development of patient pathways and public and HCP education to reduce this delay to allow the ambitious NASS Gold Standard of one year time to diagnosis to be achieved.