READ HERE
A Survey Exploring Inflammatory Back Pain in Patients With Inflammatory Bowel Disease
Jassel OK, Tahir H, Bamford S, Giuffrida P. A Survey Exploring Inflammatory Back Pain in Patients With Inflammatory Bowel Disease. Cureus. 2024 Feb 29;16(2):e55264. doi: 10.7759/cureus.55264. PMID: 38558651; PMCID: PMC10981531 A Survey Exploring Inflammatory Back Pain in Patients With Inflammatory Bowel Disease – PubMed (nih.gov)
Abstract
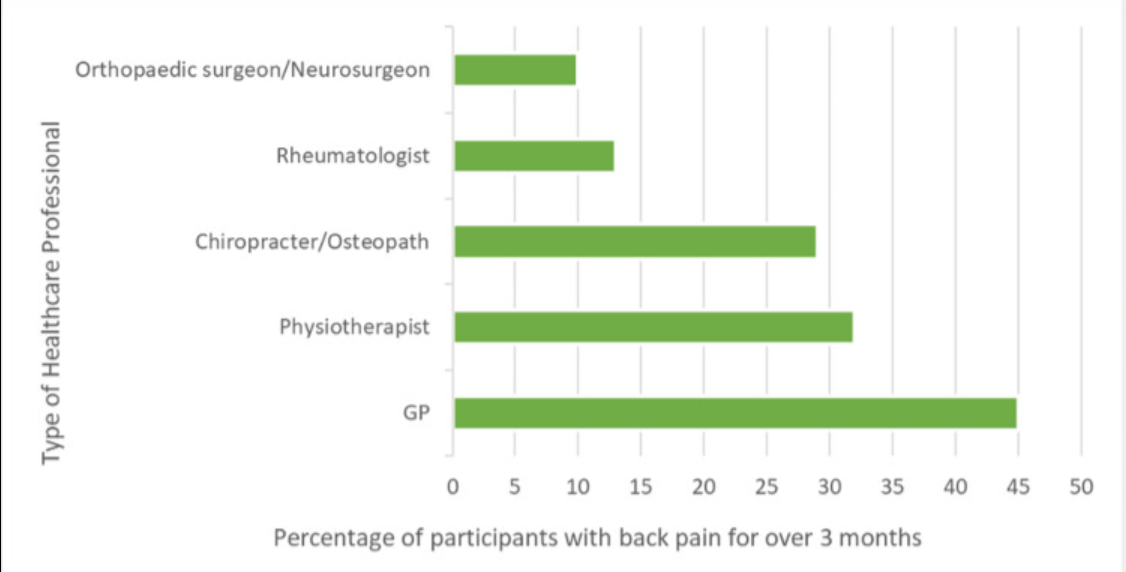
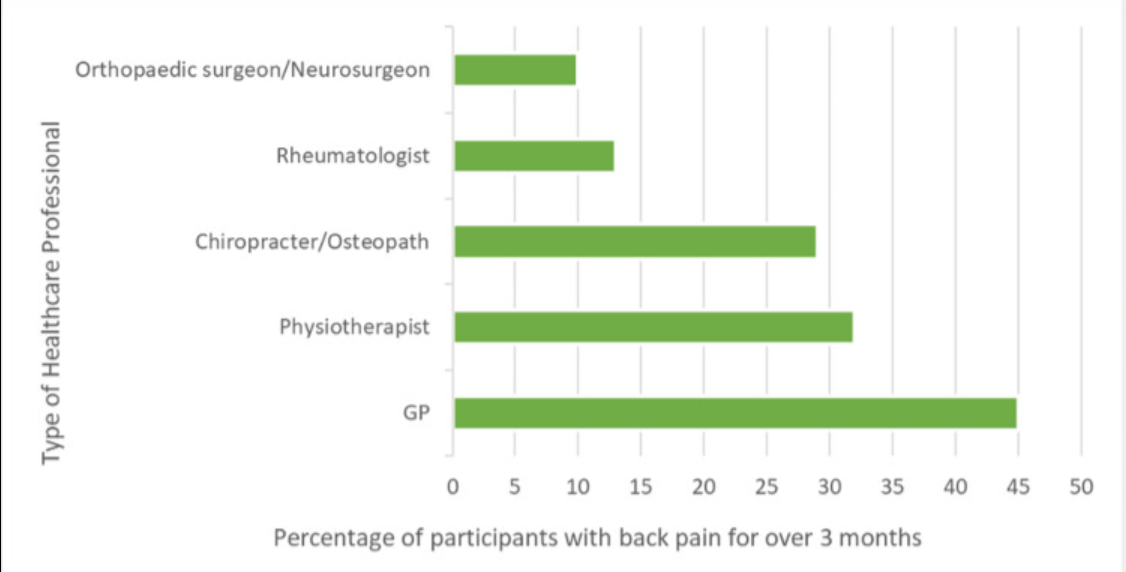
Background Diagnostic delay of axial spondyloarthritis (axSpA) is a widely recognized issue worldwide, providing a great burden for patients with this disease. AxSpA is present in a significant proportion of patients with inflammatory bowel disease (IBD). This UK study primarily aims to identify the presence of inflammatory back pain (IBP) in patients attending IBD clinic. Further aims of this study include investigating if participants had received further referrals and diagnoses for their IBP and considering factors contributing to diagnostic delay. Methods Patients were recruited from a Royal Free London NHS Trust hospital’s IBD clinic. Each participant completed a 23-question survey. The Berlin criteria were applied to the questions to investigate the presence of IBP. Further questions were asked about their IBD diagnosis and treatment, the healthcare professionals they had seen for their back pain, and other extra-articular features associated with axSpA. Results Seventy-five patients completed the online survey sent out via email. Forty percent (n = 30) of participants were female and 60% (n = 45) were male. Sixty-one percent (n = 36) of participants from the colitis clinic reported they had back pain, and 41% of the participants reported back pain for over three months. Of these, 39% (12) of participants fulfilled the Berlin criteria for IBP. Of patients experiencing back pain for over three months, we found that 10% (3) fulfilled the Berlin criteria but had not received a diagnosis for their IBP. All patients who had fulfilled the Berlin criteria but had not received a diagnosis for their IBP had seen their general practitioner (GP) and an allied healthcare professional, but not a rheumatologist. Conclusions This study highlights the presence of possibly undiagnosed axSpA in patients with IBD. The reasons for the diagnostic delay of axSpA are multifactorial. We consider specific patient characteristics, lack of awareness and education of the condition, and issues in the referral process. There is a need to improve education and awareness of axSpA, reconsider referral processes, and consider new initiatives such as joint specialty clinics to identify and treat axSpA on time.
—————————————————————————————————————————————————–
READ HERE
Identifying Axial Spondyloarthritis in Inflammatory Bowel Disease Patients Utilising Computed Tomography
Chong Seng Edwin Lim, Louise Hamilton, Samantha Bee Lian Low, Andoni Toms, Alexander Macgregor, Karl Gaffney. The Journal of Rheumatology Oct 2022, jrheum.220362; DOI: 10.3899/jrheum.220362 https://www.jrheum.org/content/early/2022/10/10/jrheum.220362
Objective
The diagnosis of axial spondyloarthritis (axSpA) is hampered by diagnostic delay. Computed Tomography (CT) undertaken for non-musculoskeletal (MSK) indications in patients with inflammatory bowel disease (IBD) offers an opportunity to identify sacroiliitis for prompt rheumatology referral. The study aims to identify what proportion of IBD patients who underwent abdominopelvic CT for non-MSK indications have axSpA and explore the role of a standardised screening tool to prospectively identify axSpA on imaging.
Methods
Abdominopelvic CT scans of verified IBD patients, age range 18-55, performed for non-MSK indications were reviewed by radiology for presence of CT-defined sacroiliitis (CTSI, using criteria from a validated CT screening tool). All patients identified were sent a screening questionnaire and those with self-reported chronic back pain (CBP), duration > 3 months, onset < 45 years were invited for rheumatology review.
Results
CTSI was identified in 60 of 301 patients. Thirty-two (53%) responded to the invitation to participate and 27 were enrolled. Of these, eight had a pre-existing axSpA diagnosis and five did not report CBP. Fourteen patients underwent rheumatology assessment; three of 14 (21.4% [95% CI: 4.7%, 50.8%]) had undiagnosed axSpA. In total, 11 of 27 (40.7% [95% CI: 22.4%, 61.2%]) patients had a rheumatologist verified diagnosis of axSpA.
Conclusion
At least 5.0% of IBD patients (3/60) undergoing abdominopelvic CT for non-MSK indications with CTSI have undiagnosed axSpA, and overall, 18.3% (11/60) have axSpA. This reveals a significant hidden population of axSpA and highlights the need for a streamlined pathway from sacroiliitis detection to rheumatology referral.
—————————————————————————————————————————————————–
READ HERE
Prevalence of undiagnosed axial spondyloarthritis in inflammatory bowel disease patients with chronic back pain: secondary care cross-sectional study.
Chong Seng Edwin Lim, Mark Tremelling, Louise Hamilton, Matthew Kim, Alexander Macgregor, Tom Turmezei, Karl Gaffney, Prevalence of undiagnosed axial spondyloarthritis in inflammatory bowel disease patients with chronic back pain: secondary care cross-sectional study, Rheumatology, 2022;, keac473, https://doi.org/10.1093/rheumatology/keac473
Objective
To elucidate the prevalence of undiagnosed rheumatologist-verified diagnosis of axial spondyloarthritis (RVD-axSpA) in patients attending routine secondary care IBD clinics with chronic back pain.
Methods
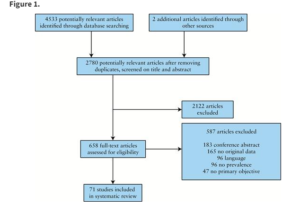
Screening questionnaires were sent to consecutive patients attending IBD clinics in a university teaching hospital. Patients fulling the eligibility criteria (gastroenterologist-verified diagnosis, 18–80 years old, biologic therapy naïve, no previous diagnosis of axSpA); and a moderate diagnostic probability of axSpA (self-reported chronic back pain [CBP] > 3 months, onset < 45 years) were invited for rheumatology assessment. This included medical review, physical examination, patient reported outcome measures, human leucocyte antigen B27, C-reactive protein, pelvic radiograph and axSpA protocol magnetic resonance imaging. A diagnosis of RVD-axSpA was made by a panel of rheumatologists.
Results
Of the 470 patients approached, 91 had self-reported CBP > 3 months, onset < 45 years, of whom 82 were eligible for clinical assessment. The prevalence of undiagnosed RVD-axSpA in patients attending IBD clinics in a secondary care setting, with self-reported CBP, onset < 45 years is estimated at 5% (95% CI 1.3,12.0) with a mean symptom duration of 12 (S.D. 12.4) years.
Conclusion
There is a significant hidden disease burden of axSpA among IBD patients. Appropriate identification and referral from gastroenterology is needed to potentially shorten the delay to diagnosis and allow access to appropriate therapy.