READ HERE
Evaluation of the current use of MRI to aid the diagnosis of axial spondyloarthritis in the UK: results from a freedom of information request
Bray TJP et al., Evaluation of the current use of MRI to aid the diagnosis of axial spondyloarthritis in the UK: results
from a freedom of information request, Clinical Radiology, https://doi.org/10.1016/j.crad.2023.10.009
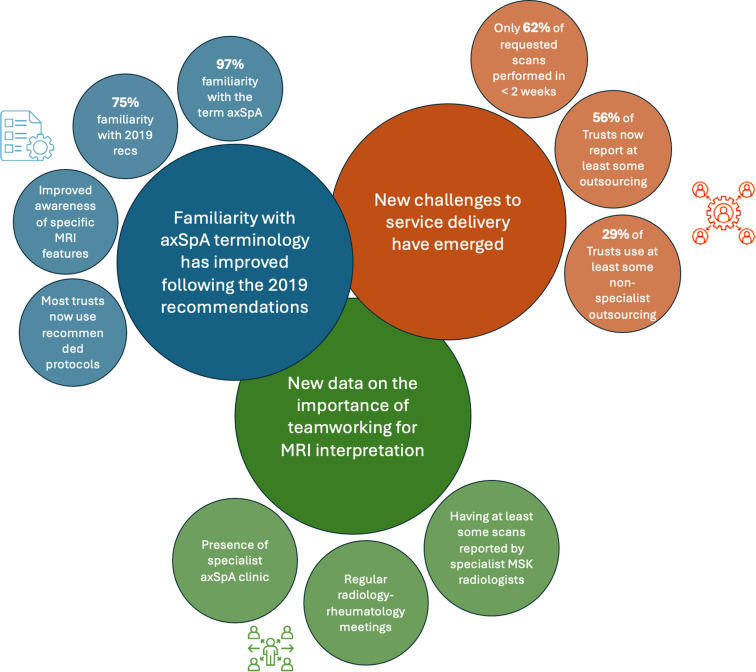
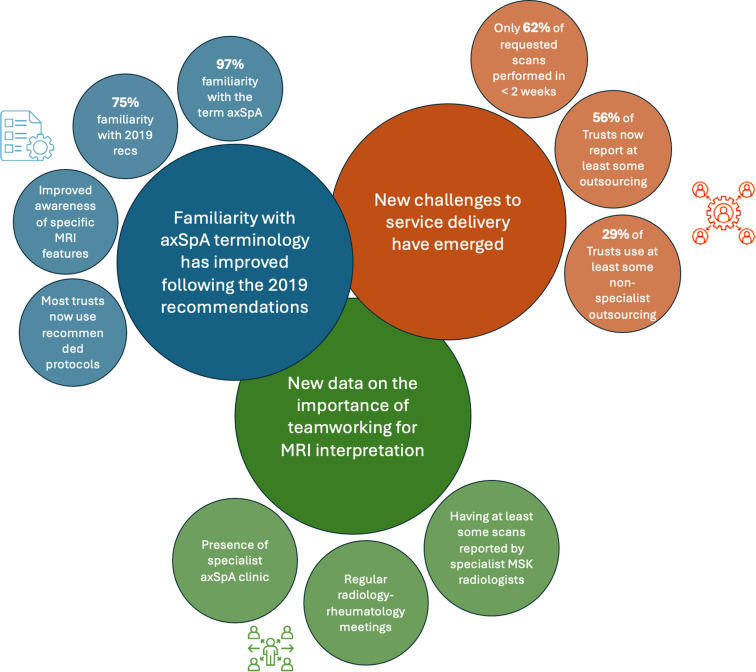
- AIM: To evaluate the impact of recommendations from the 2019 consensus exercise conducted by radiologists and rheumatologists on the use of magnetic resonance imaging (MRI) to investigate axial spondyloarthritis (axSpA) in clinical practice.
- MATERIALS AND METHODS: A freedom of information (FOI) request was used to assess the use of MRI in the diagnosis of axSpA and radiologists’ awareness of the 2019 guidance across all NHS Trusts and Health Boards in the UK, including England, Scotland, Northern Ireland, and Wales.
- RESULTS: The FOI request was sent to 150 Trusts/Health Boards, and 93 full responses were received. Of the 93 respondents (97%), 90 reported familiarity with the term axSpA and 70/93 (75%) reported familiarity with the 2019 recommendations. Awareness of recommendations regarding specific MRI features supportive of the diagnosis of axSpA was 74/93 (80%) for the sacroiliac joints (SIJs) and 66/93 (71%) for the spine. The median wait for MRI acquisition was 2 e3 months. Fifty-two of the 93 (56%) reported at least some outsourcing of axSpA MRI (33%/29% for specialist/non-specialist outsourcing respectively); 32/93 (34%) reported some scans being reported in-house by non- musculoskeletal radiologists.
- CONCLUSION: There have been several positive developments in the understanding and use of MRI for the diagnosis of axSpA in the UK since the 2017 survey, although substantial scope for further improvement remains. Several new challenges have also emerged, including the
———————————————————————-

READ HERE
MRI lesions of the spine in patients with axial spondyloarthritis: an update of lesion definitions and validation by the ASAS MRI working group
Baraliakos X, Østergaard M, Lambert RG, et al. MRI lesions of the spine in patients with axial spondyloarthritis: an update of lesion definitions and validation by the ASAS MRI working group.
Annals of the Rheumatic Diseases Published Online First: 24 May 2022. doi: 10.1136/annrheumdis-2021-222081
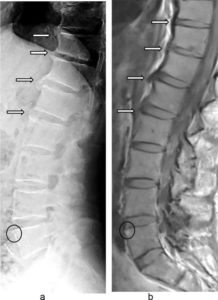
Objectives Spinal MRI is used to visualise lesions associated with axial spondyloarthritis (axSpA). The ASAS MRI working group (WG) updated and validated the definitions for inflammatory and structural spinal lesions in the context of axSpA.
Methods After review of the existing literature on all possible types of spinal MRI pathologies in axSpA, the group (12 rheumatologists and two radiologists) consented on the required revisions of lesion definitions compared with the existing nomenclature of 2012. In a second step, using 62 MRI scans from the ASAS classification cohort, the proposed definitions were validated in a multireader campaign by global (absent/present) and detailed (inflammation and structural) lesion assessment at the vertebral corner (VC), vertebral endplate, facet joints, transverse processes, lateral and posterior elements. Intraclass correlation coefficient (ICC) was used for analysis.
Results Revisions were made for both inflammatory (bone marrow oedema, BMO) and structural (fat, erosion, bone spur and ankylosis) lesions, including localisation (central vs lateral), extension (VC vs vertebral endplate) and extent (minimum number of slices needed), while new definitions were suggested for the type of lesion based on lesion maturity (VC monomorphic vs dimorphic). The most reliably assessed lesions were VC fat lesion and VC monomorphic BMO (ICC (mean of all 36 reader pairs/overall 9 readers): 0.91/0.92; 0.70/0.67, respectively.
Conclusions The lesion definitions for spinal MRI lesions compatible with SpA were updated by consensus and validated by a group of experienced readers. The lesions with the highest frequency and best reliability were fat and monomorphic inflammatory lesions at the VC.
READ HERE
Deep learning algorithms for magnetic resonance imaging of inflammatory sacroiliitis in axial spondyloarthritis
Karina Ying Ying Lin, Cao Peng, Kam Ho Lee, Shirley Chiu Wai Chan, Ho Yin Chung, Deep learning algorithms for magnetic resonance imaging of inflammatory sacroiliitis in axial spondyloarthritis, Rheumatology, 2022;, keac059, https://doi.org/10.1093/rheumatology/keac059
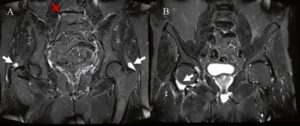
Objective: The aim of this study was to develop a deep learning algorithm for detection of active inflammatory sacroiliitis in short tau inversion recovery (STIR) sequence MRI.
Results: Inflammatory sacroiliitis was identified in 1398 MR images from 228 participants. No inflammation was found in 3944 MRI scans from 161 participants. The mean sensitivity of the algorithms derived from the original dataset and fake-colour image dataset were 0.86 (0.02) and 0.90 (0.01), respectively. The mean specificity of the algorithms derived from the original and the fake-colour image datasets were 0.92 (0.02) and 0.93 (0.01), respectively. The mean testing dice coefficients were 0.48 (0.27) for the original dataset and 0.51 (0.25) for the fake-colour image dataset. The area under the curve of the receiver operating characteristic (AUC-ROC) curve of the algorithms using the original dataset and the fake-colour image dataset were 0.92 and 0.96, respectively. The sensitivity and specificity of the algorithms were comparable with the interpretation by a radiologist, but outperformed that of the rheumatologist.
Conclusion: An MRI deep learning algorithm was developed for detection of inflammatory sacroiliitis in axial SpA.