READ HERE
Patient Survey Exploring the Burden of Inflammatory Back Pain in Patients With Uveitis
Bamford S, Tahir H, Ladan Z, et al. (April 12, 2023) Patient Survey Exploring the Burden of Inflammatory Back Pain in Patients With Uveitis.
Cureus 15(4): e37473. DOI 10.7759/cureus.37473
Background
In the UK, diagnostic delays remain a challenge in axial spondyloarthritis (axSpA). Studies have shown that acute anterior uveitis is the most common extra-articular manifestation associated with axSpA. As part of a National Axial Spondyloarthritis Society (NASS) Aspiring to Excellence quality improvement project, this study aimed to ascertain the burden of inflammatory back pain (IBP) in patients attending a uveitis clinic and to establish the number of these patients who had not been referred to a rheumatologist, thereby contributing to the diagnostic delay. The secondary aims were to explore the factors contributing to the diagnostic delay.
Methods
A 22-question patient survey was created to identify the burden of back pain in patients attending as pecialist uveitis clinic at a London NHS Trust. Participants were recruited when attending their clinic appointments. Survey content included patient demographics and whether they had experienced back pain for longer than three months. The Berlin Criteria was used to identify the presence of inflammatory back pain, and it was also ascertained whether participants had a previous diagnosis of axSpA. Participants were asked if they had seen any healthcare professionals regarding their back pain and the total number of consultations they had had with each profession.
Results
A cohort of 50 patients who attended the uveitis clinic at the Royal Free London NHS Trust completed the survey between February and July 2022. The mean age of the respondents was 52 years with a mean length of time with uveitis of 6.57 years. Of them, 64% were female and 36% were male. Forty per cent (40%) of participants (20 respondents) reported experiencing back pain for more than three months and 12% (six respondents) had a diagnosis of axSpA. Of those who reported back pain for more than three months, the mean age of onset of back pain was 28.6 years. Of the 14 participants (28%) who had back pain and were not diagnosed with axSpA, nine (18%) fulfilled the Berlin criteria for IBP. All participants had seen a GP or allied health professional specifically for their back pain. On average, respondents had seen two allied healthcare professionals, but only 40% (eight) of respondents with back pain had been seen by a rheumatologist.
Conclusions
In this study, the data highlights that inflammatory back pain is common in patients with uveitis and the majority of patients with inflammatory back pain had not been referred to a rheumatology service and potentially have undiagnosed axSpA. Contributing factors to this potential delay in diagnosis include a lack of awareness of axSpA and its presenting features and associated conditions and a lack of onward referral for a specialist rheumatology opinion. This highlights the need for public, patient and healthcare professional education and the development of timely referral pathways to reduce delays in diagnosis.
———————————————————————————————————————————————————————-
READ HERE
Prevalence of axial spondyloarthritis in patients with acute anterior uveitis: a cross-sectional study utilising MRI.
Sykes MP, Hamilton L, Jones C, Gaffney K. Prevalence of axial spondyloarthritis in patients with acute anterior uveitis: a cross-sectional study utilising MRI. RMD Open. 2018;4(1):e000553. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5845401/
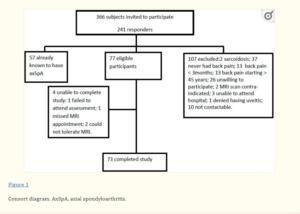
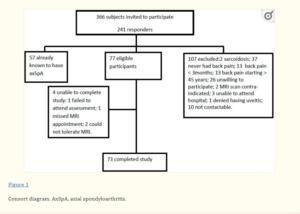
AAU is known to be the most common EAM of axial SpA. In this study, the minimum prevalence of axial SpA in AAU was 20.2%; nearly one-quarter of these patients previously undiagnosed despite years of back pain – representing a substantial hidden burden of disease. HLA-B27 diagnosis is often the trigger for referral of patients with AAU to rheumatology. However, nearly one-half of patients identified as missed diagnoses were HLA-B27 negative. Similarly, nearly two-thirds of new diagnoses would have been missed if using inflammatory back pain rather than chronic back pain as a referral strategy – supporting the presence of inflammatory back pain as an axial SpA feature rather than mandatory criterion for referral, in line with Assessment of Spondyloarthritis International Society (ASAS)-endorsed recommendations for early referral. Due to the high prevalence of axial SpA among individuals presenting with AAU, the authors thereby recommend that all individuals with AAU and chronic back pain with onset before the age of 45 should be referred to rheumatology regardless of HLA-B27 status, gender or number of episodes of AAU.