READ HERE
A UK survey evaluation of First Contact Practitioners’ and musculoskeletal physiotherapists’ confidence, recognition, and referral of suspected axial spondyloarthritis
Steen, E., McCrum, C., & Cairns, M. (2022). A UK survey evaluation of First Contact Practitioners’ and musculoskeletal physiotherapists’ confidence, recognition, and referral of suspected axial spondyloarthritis. Musculoskeletal Care, 1– 17. https://doi.org/10.1002/msc.1706
Background
Axial Spondyloarthritis is an inflammatory disease associated with significant diagnostic delays. Steen et al. (2021) found inadequate consideration of axial Spondyloarthritis (axSpA) in physiotherapists back pain assessments. Since the previous survey, increased professional education on axSpA has occurred and First Contact Practitioners (FCPs), now widely established in General Practice, are key in supporting earlier recognition.
Objectives
(1) To re-evaluate physiotherapists’ and evaluate FCPs’ awareness, knowledge, and confidence in screening for and recognising features of axSpA and criteria prompting referral to rheumatology. (2) To compare these results to previous research (Steen et al., 2021).
Design
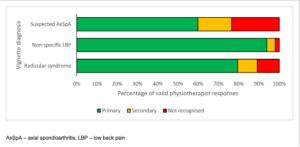
As per Steen et al. (2021), an online survey was undertaken combining back pain vignettes (reflecting axSpA, non-specific low back pain [NSLBP] and radicular syndrome) and questioning on features of suspected axSpA.
Results
165 surveys were analysed. Only 73% (n = 120/165) of respondents recognised the axSpA vignette compared to NSLBP 91% (n = 80/88) and radicular syndrome 88% (n = 68/77). An improvement in axSpA recognition was demonstrated compared with previous data. FCPs performed slightly better with 77% (n = 67/87) of respondents recognising the axSpA vignette. Adequate awareness of national referral guidance was evident in only 55% of ‘clinical reasoning’ and 6% of ‘further subjective screening’ responses. There was still misplaced confidence in recognising clinical features of axSpA compared to knowledge levels shown, including high importance given to inflammatory markers.
Conclusion(s)
Musculoskeletal physiotherapists demonstrate some improved knowledge and awareness of axSpA compared with previous study findings. Consideration of axSpA is still not universal in musculoskeletal physiotherapists’ or FCPs’ approaches to persistent back pain assessments and awareness of national referral guidance remains limited. This study highlights the continued need for professional education. Enhanced knowledge of screening and referral criteria in musculoskeletal clinical practice would support earlier diagnosis and better outcomes.