How to recognise axial spondyloarthritis in dermatology
Although screening tools such as PEST (Psoriasis Epidemiology Screening Tool) are extremely useful, they won’t always pick up the early signs of axial SpA, due to the fact that back pain often gets overlooked by dermatologists. Given lower back pain is one of the key symptoms synonymous with axial SpA, particularly in younger cohorts aged <45 years, it needs to be higher on the radar of dermatologists seeing patients with psoriasis.
NASS has developed a screening tool to indicate when onward referral to rheumatology is appropriate.
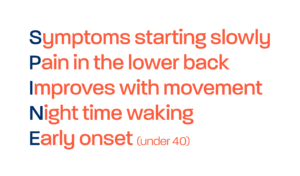
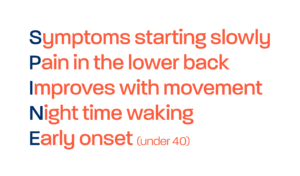
So when should you consider axial SpA?
If a patient less than 45 years old presents to your clinic with psoriasis but with no diagnosis of axial SpA, you can ask them whether they experience back pain. If this pain has persisted for over 3 months, then you should ask the following screening questions:
- Did your back pain develop gradually?
- Do you experience stiffness in your back in the morning for at least 30 minutes?
- Does your back pain improve when you move around?
- Do you have pain in your buttocks, which moves from one buttock to the other?
- Do you wake in the second half of the night because of your back pain?
If answering “Yes” to 3 or more of the above, then the patient meets criteria for inflammatory back pain and could have axial SpA. In that case the recommendation is for you to refer urgently, directly to rheumatology. This can be done via an internal tertiary referral pathway at your hospital.
We encourage you to utilise the above screening tool in your next clinic, when a patient aged <45 presents with psoriasis and persistent lower back pain; to help reduce delay to diagnosis in axial SpA.
If you feel that your service could benefit from support in improving awareness of axial SpA, or improving use or availability of internal tertiary referral pathways, then please reach out to the Gold Standard Team at goldstandard@nass.co.uk .