Although acute anterior uveitis (AAU) is a relatively rare inflammatory eye condition, we know that up to 26% of people with diagnosed axial spondyloarthritis (axial SpA) live with the condition. We also know from an algorithm developed to predict axial SpA in people with AAU, that as many as 30% of people with AAU may be living with undiagnosed axial SpA.
Given that AAU is an extra-articular manifestation of axial SpA, specialists in ophthalmology therefore have a key role to play in screening undiagnosed patients for urgent referral to rheumatology.
Dr Fahd Quhill is a University Senior Lecturer and Consultant Ophthalmologist at Sheffield Teaching Hospitals NHS Foundation Trust and Royal Hallamshire Hospital. Below, Fahd provides an overview of key symptoms to look out for when considering axial SpA in ophthalmology, in addition to advice on when to refer to rheumatology.
How to recognise axial SpA in ophthalmology
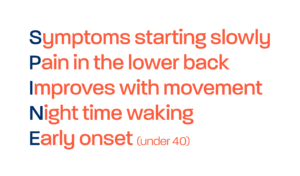
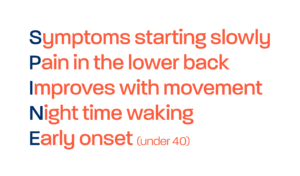
The key to this screening is really about understanding why diagnosis is missed. Axial SpA is an inflammatory arthritis of the spine, often presenting in individuals in their late teens, early 20’s and 30’s. Presentation can vary from patient to patient, but one of the key symptoms is chronic lower back pain. Other symptoms can include fatigue, morning stiffness and reduced mobility. In addition to other extra-articular manifestations including psoriasis and inflammatory bowel disease. With such a young age of onset and variety of symptoms that can come and go over time as the disease progresses, the individual can end up consulting a range of specialists for individual symptoms and care, without the dots being connected. Primary care may not have identified inflammatory back pain, or a referral to physiotherapy or a pain clinic may still have left the underlying axial SpA undiagnosed.
With the Gold Standard Time to Diagnosis programme, NASS hope to raise awareness of axial SpA in secondary care specialties that treat extra articular manifestations such as ophthalmology, to ensure earlier referral and treatment of axial SpA. We hope that this video can encourage you to also include axial SpA and its symptoms in your clinical reasoning, to improve direct referrals of suspected axial SpA from ophthalmology to rheumatology.
So when should you consider axial SpA?
If a patient less than 45 years old presents to your clinic with AAU but with no diagnosis of axial SpA, you can ask them whether they experience lower back pain. If this pain has persisted for over 3 months, then you should refer urgently directly to rheumatology. This can be done via an internal tertiary referral pathway at your hospital.
If you feel that your service could benefit from support in improving awareness of axial SpA, or improving use or availability of internal tertiary referral pathways, then please reach out to the Gold Standard Team at goldstandard@nass.co.uk.