Recognising axial SpA: top tips!
1. CONSIDER INFLAMMATORY BACK PAIN HISTORY
Although axial SpA is associated with inflammatory back pain, some patients with axial SpA may present with mechanical sounding pain: including lower back pain, radiating buttock pain, or sometimes even thigh pain anterior or posterior to the knee. It is therefore important to enquire about prior episodes of back pain, as often axial SpA patients will experience multiple episodes of back pain which come and go or are eased with NSAIDs. This could be mistaken for a natural healing process associated with mechanical back pain, when in fact it could be intermittent episodes of flare or inflammation.
2. ASK ABOUT SLEEP
A good indication of inflammatory back pain is night pain or waking in the second half of the night due to pain, whereby patients are then unable to get back to sleep. Many patients with axial SpA describe being disturbed in the night due to pain, thereby needing to get up and walk around in the night or take painkillers in order to go back to sleep. Asking about sleep can therefore give a good indication of the nature of the back pain. Similarly, presentations of alternating buttock pain should always raise suspicion of an inflammatory condition.
3. CONSIDER RESPONSE TO NSAIDS
Many patients with inflammatory back pain will respond well to NSAIDs. Prior NSAID response can therefore be indicative of inflammatory back pain. If appropriate, you may need to guide your patients to seek GP review to consider a course of NSAIDs if they have not previously tried them.
4. ASK ABOUT THE EXTRA-ARTICULAR MANIFESTATIONS OF AXIAL SPA
Axial SpA is associated with a range of extra-articular manifestations, or EAMs, including acute anterior uveitis, psoriasis, and inflammatory bowel disease (ulcerative colitis and Crohn’s disease) – conditions associated with the eyes, skin, and bowels, respectively. Dactylitis and enthesitis are also EAMs of axial SpA. Presence or prior bouts/ history of these conditions could indicate that a patient’s back pain is more likely to be inflammatory or axial SpA related. For example, history of a one off knee effusion, episode of uveitis or a previous gastrointestinal infection may all prove important information for you & raise your level of suspicion.
5. ASK ABOUT OTHER FAMILY MEMBERS
As there may be a family link in axial SpA, ascertaining if anyone in your patients’ immediate family circle has had axial SpA, inflammatory back pain or any of the EAMs mentioned above could prove to be important information. If yes, this could raise the probability of your patients’ symptoms being inflammatory in nature.
6. BE AWARE OF INFLAMMATORY BACK PAIN IN FEMALES
Historically, axial SpA was considered a predominantly male disease, likely due to the fact that radiographic axial SpA, or ankylosing spondylitis, is more common in males. However, with the advent of MRI to identify earlier inflammatory changes, we now know that non-radiographic axial SpA is just as common in females. It is therefore important to move away from just thinking of axial SpA solely as ankylosing spondylitis, identified by X-ray changes to the spine, and instead consider the wider net of people with non-radiographic axial spondyloarthritis also. These patients may present with a variety of symptoms – but the key feature is chronic back pain with onset aged <45 years.
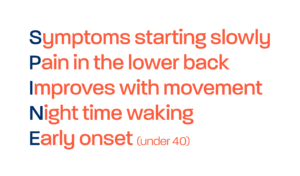
7. USE THE SPADE TOOL
The SPADE tool is a quick and easy resource that can help you determine whether referral to rheumatology is necessary, based on present symptoms. Visit our page on the SPADE tool. Being aware of NICE guidance is also critical.
8. KNOW YOUR LOCAL RHEUMATOLOGY PATHWAYS
It is really important that you understand the appropriate pathways to rheumatology services in your area, as this may vary depending on where you are in the UK. Contact, reach out and link with your local rheumatology services. It will always prove really helpful if you can gain advice and guidance from the rheumatology consultant or local rheumatology team on any suspicious cases. Also, find out what they do/do not like physiotherapists to do and their expectations for referral. For example, blood tests can help build up a clinical picture of potential axial SpA. However, some rheumatology services may prefer that you refer directly to rheumatology, without performing any further tests or investigations in primary care, e.g. blood tests for HLA-B27, CRP or ESR, which are not diagnostic for axial SpA, but may help with determining your index of suspicion of axial SpA*.
*Notes:
- HLA-B27 is not diagnostic of axial SpA, but a large proportion of people with axial SpA will be positive for this blood test. Approximately 8% of white western Europeans carry this gene, in comparison to 75-90% of individuals with axial SpA. However, only about 1 in 15 people who are HLA-B27 positive go on to develop the condition. Over 100 genes are now thought to be involved in axial SpA, with HLA-B27 believed to be responsible for no more than 25-30% of the genetic risk.
- Similarly, CRP or ESR is not diagnostic of axial SpA. But elevated CRP/ESR can be an indicator of inflammation.
Know your axial spondyloarthritis features, ask the appropriate questions, and refer early to rheumatology. This way, we can really help reduce delay to diagnosis in these conditions, to ultimately improve outcomes for our patients.