READ HERE
Classification vs diagnostic criteria: the challenge of diagnosing axial spondyloarthritis.
Poddubnyy D. Classification vs diagnostic criteria: the challenge of diagnosing axial spondyloarthritis. Rheumatology. 2020;59(Supplement_4):iv6-iv17. https://doi.org/10.1093/rheumatology/keaa250
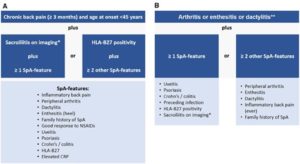
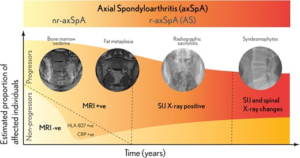
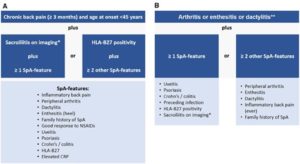
In recent years, significant progress has been made in improving the early diagnosis of spondyloarthritides (SpA), including axial SpA. Nonetheless, there are still issues related to the application of classification criteria for making the primary diagnosis of SpA in the daily practice. There are substantial conceptional and operational differences between the diagnostic vs classification approach. Although it is not possible to develop true diagnostic criteria for natural reasons as discussed in this review, the main principles of the diagnostic approach can be clearly defined: consider the pre-test probability of the disease, evaluate positive and negative results of the diagnostic test, exclude other entities, and estimate the probability of the disease at the end. Denis Poddubnyy describes the diagnostic process as a “diagnostic scale”, whereby one should weigh positive test results and present clinical features against negative test results and the presence of an alternative explanation for the symptoms. Even when all tests have been conducted, a diagnosis of axial SpA may remain uncertain. However, we know that these conditions change and evolve over time. If a diagnosis of axial SpA cannot be confirmed but clinical suspicion remains high, consider a follow‑up MRI to monitor for any potential future inflammatory changes. Classification criteria should only be applied to patients with an established diagnosis and aimed at the identification of a homogeneous group of patients for the conduction of clinical research.