James Holland NASS Champion in Primary Care shares tips for First Contact Physiotherapists on how to identify and diagnose axial SpA (or axSpA, including Ankylosing Spondylitis or AS) including solutions
James provides an overview of the importance of improved diagnosis in axial SpA, in addition to providing tips for recognising axial SpA for first contact physiotherapists (FCP), and gives an overview of some of the solutions being developed by the NASS Champions in Primary Care.
Top tips for FCPs for axial SpA diagnosis
1. Utilise the ASAS criteria and questions
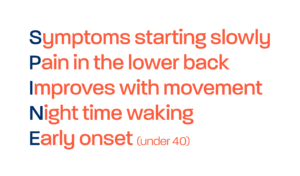
ASAS have an inflammatory back pain questionnaire, which covers five questions. It is important to ask patients coming to see you with back pain. First of all, age is an important feature, due to early onset of symptoms, with axSpA affecting younger people, typically under the age of 40. Patients with inflammatory back pain tend to report to being better when they exercise, and worse when they are resting or immobile. Patients often experience night pain in the second half of the night which is enough to get them out of bed.
If a patient answers yes to 4 or more of the following 5 questions, they have an approximately 80% chance of having inflammatory back pain.
- Did back pain start before the age of 40?
- Was the onset of pain gradual?
- Does the pain get better with exercise?
- Does the pain get worse, or not improve, with rest?
- Does the back pain cause waking in the second half of the night, requiring the individual to move around before feeling better and being able to fall asleep?
2. ASK about Extra Musculoskeletal Manifestations (EMM) or linked conditions
You need to understand if there are other features of inflammatory conditions in their medical history, such as psoriasis, inflammatory bowel disease, such as Crohn’s and Colitis and Uveitis. It is really important to be thinking of those linked conditions as they can indicate axSpA or raise additional suspicion.
3. Utilise technology – such as pop ups or templates
In Stockport we have developed a pop up tool within the EMIS primary care system which helps to identify potential inflammatory back pain. It will identify patients between the age of 18 and 45 that have had an episode of back pain in the past 12 months when they come to the practice. It looks for any inflammatory conditions in the patients medical record, for CRP and other genetical blood tests like HLAB27, and pop up to suggest that you consider inflammatory back pain and link to the 5 ASAS questions and the SPADE tool.
4. Coding
The tools such as the pop up will only work if episodes of care are appropriately coded. It is able to identify previous back pain, prescence of EMMs and various tests that will help you to build a clinical picture. If patients are not coded appropriately for the issue they present with or conditions they live with it will hinder such tools. So coding properly is imperative.
Know your axial spondyloarthritis features, ask the appropriate questions, and refer early to rheumatology. This way, we can really help reduce delay to diagnosis in these conditions, to ultimately improve outcomes for our patients.